Bacterial Pathogenesis
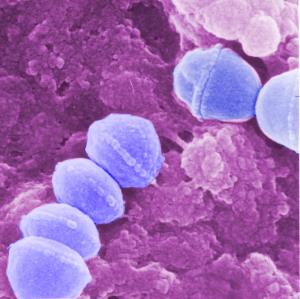
GAS Pathogenesis
Group A Streptococcus (GAS) is an important human pathogen causing diseases ranging from simple pharyngitis ("strep throat") to invasive necrotizing fasciitis ("flesh-eating disease") to the immune-mediated syndrome of rheumatic fever. Our lab aims to discover and characterize GAS virulence factors by coupling genetic approaches (e.g. targeted mutagenesis) with tissue culture and murine infection models. Of particular interest are genetic mechanisms of GAS innate immune resistance and the shift from mucosal colonization to systemic disease. Among the GAS virulence factors we study are the pore-forming toxins streptolysins S and O (SLS and SLO), the antiphagocytic and proinflammatory surface M protein, DNAse Sda1, cysteine protease SpeB, hyaluronic acid capsule, serum opacity factor, IL-8 peptidase, and the cell wall group A carbohydrate. Together, these studies aim to provide new targets for drug therapy and vaccine prophylaxis. Our collaborators include M. Walker (U. Queensland), P. Ghosh (UCSD), J. Dixon (UCSD), M. Kotb (Cincinnati) and E. Hanski (Jerusalem).
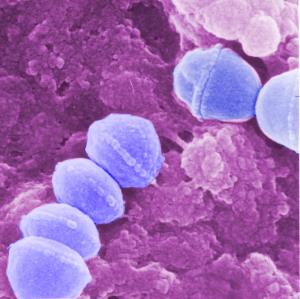
GBS Pathogenesis

Group B Streptococcus (GBS) is the leading cause of invasive bacterial infections in human newborn infants, including pneumonia, sepsis and meningitis. GBS is also increasingly associated with severe infections in nonpregnant adults, especially those with underlying diseases that weaken immunity. Our laboratory has studied several aspects of GBS pathogenesis through random transposon and allelic exchange mutagenesis paired with in vitro cell culture models and in vivo small animal challenges. Major areas of investigation have include the molecular genetics and virulence properties of the GBS pore-forming hemolysin/cytolysin toxin, functions of the sialic acid-expressing GBS polysaccharide capsule in molecular mimicry and evasion of innate immune clearance, mechanisms of lung injury and inflammatory responses in GBS pneumonia in the premature infant, the role of GBS surface proteins and cell wall components in cellular adherence and invasion, and the molecular basis of GBS penetration of and injury to the blood-brain barrier endothelium in the pathogenesis of newborn meningitis. Our collaborators include Kelly Doran (SDSU) and Ajit Varki (UCSD).
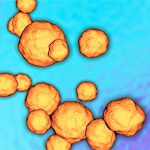
S. aureus Virulence
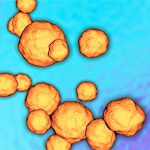
Staphylococcus aureus causes nosocomial and community-acquired diseases including skin and soft tissue infections, osteomyelitis, bacteremia, abscesses, endocarditis and septicemia. Antibiotic resistance has reached epidemic proportions in many regions, with methicillin-resistant S. aureus (MRSA) now exceeding HIV/AIDS as a cause of death in the U.S. Our S. aureus research includes study of how the pathogen resists killing by human phagocytes, including the antioxidant properties of its golden carotenoid pigment, staphyloxanthin. Pigment inhibition, achieved through repurposing of human cholesterol-lowering agents, may hold promise as an adjunct to antibiotic therapy of MRSA. Other immune evasion factors under investigation include S. aureus nitric oxide synthase, phenol soluble modulins, Ig-binding protein A and the pore-forming α-hemolysin. We are also investigating S. aureus colonization and skin infection, to better understand how the pathogen both activates and resists cutaneous innate defenses. Our collaborators include George Liu (UCSD), Eric Oldfield (U. Illinois), Pieter Dorrestein (UCSD), Suzan Roiijakkers (Utrecht) and AuricX Pharmaceuticals (Houston).
S. pneumoniae Pathogenesis

Streptococcus pneumoniae (SPN) is perhaps the leading cause of clinically significant bacterial infections worldwide, with a disease spectrum ranging from simple otitis media and sinusitis to invasive conditions including pneumonia, sepsis and meningitis. We have been interested in multiple roles of the surface-anchored pneumococcal neuraminidase (sialidase), NanA, in disease pathogenesis. In addition to its ability to cleave terminal sialic acid motifs on host cell targets, we have shown that an additional domain of the protein promotes invasion of brain microvascular endothelial cells and the development of pneumococal meningitis. Also, by cleaving sialic acid from host cell surfaces, the tonic engagement in cis of inhibitory Siglec receptors is released, leading to exaggerated leukocyte inflammatory responses. Finally, we have studied how NanA sialidase modifies platelets and clotting factors to promote their clearance by the hepatic Ashwell receptor, influencing the development of disseminated intravascular coagulation during pneumococcal sepsis. Our collaborators include Ajit Varki (UCSD), David Gonzalez (UCSD), Jamey Marth (SBMRI), and Kelly Doran (SDSU).
Multidrug Resistant Gram-negative Bacteria

Multidrug resistant (MDR) bacterial infections are an urgent threat to human health and predicted to cause 10 million deaths annually by the year 2050. Six ESKAPE pathogens are designated by the World Health Organization and Centers for Disease Control as key targets for novel therapeutic development due to the lack of effective interventions and their propensity to rapidly acquire resistance. We investigate virulence and resistance mechanisms by Acinetobacter baumannii, Pseudomonas aeruginosa, Klebsiella pneumonaie, E coli, and other clinically relevant ESKAPE pathogens. We harness our knowledge of critical virulence factors to test suitable antigens for vaccine candidates and novel biotherapeutics. Our collaborators include George Liu (UCSD).
Other areas of research: