Innate Immunity
Neutrophil Extracellular Traps (NETs)

Neutrophil extracellular traps (NETs) consist of nuclear (or mitochondrial) DNA as a backbone with embedded antimicrobial peptides, histones, and cell-specific proteases providing a matrix to entrap and kill microbes. NETs are formed after stimulation with mitogens, cytokines, or pathogens themselves, in a specialized cell death process involving a ROS-mediated signaling cascade and particular chromatin modifications. We are exploring roles of HIF-1α and cathelicidins in the generation of NETs at peripheral foci of infection, and have uncovered a novel contribution of the cholesterol biosynthetic pathway in the regulation of NET formation. We are also investigating other immune cells including mast cells and macrophages can themselves produce extracellular traps to control pathogens. Companion projects examine how specific bacterial factors (e.g. GAS M protein) stimulate NET production, whereas other virulence factors promote bacterial resistance to NET killing, e.g. by degradation of the NET architecture (DNAses of GAS and S. aureus) or resistance to the embedded cathelicidins. Collaborators include Maren von Köckritz-Blickwede (Hannover).
Host-Pathogen Glycobiology

The surface of all bacterial and human cells are covered with glycan molecules that play a primary role in arbitrating the outcome of the host-pathogen encounter. We are members of the UCSD Program in Excellence in Glycosciences (PEG) and Glycobiology Research and Training Center (GRTC) spearheading collaborative projects that examine the role of bacterial glycans and glycosidases in modulating myeloid cell innate immune and inflammatory responses. One major focus is the role of sialic acid binding lectins known as Siglecs in regulation of leukocyte function, and their subversion through molecular mimicry by GBS expressing its sialylated polysaccharide capsule. We are also studying the role of GAS hyaluronic acid in interactions with CD44, proinflammatory effects of bacterial sialidases and hyaluronidases, the role of host glycosaminoglycans in neutrophil and endothelial barrier function during infection, and the potential of reprogramming natural antibodies against the nonhuman αGal epitope to clear drug-resistant pathogens via engineered RNA aptamers. Collaborators include A. Varki (UCSD), J. Esko (UCSD), R. Gallo (UCSD) and Altermune Technologies (London).
Platlets as Immune Mediators
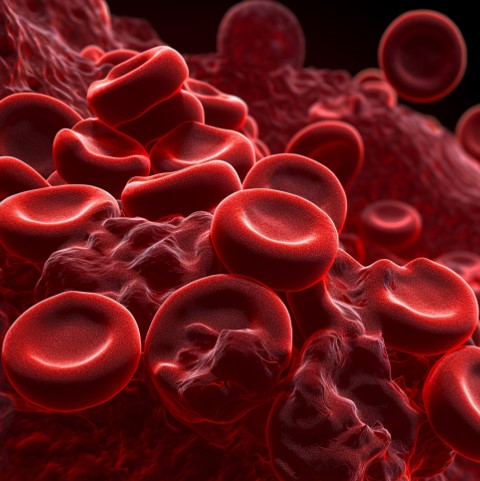
Platelets, small anuclear circulating cells, are well known for their role in hemostasis. More recently, platelets have been identified as critical immune mediators in response to bacterial pathogens. Our focus examined the role of platelets during
Staphylococcus aureus infection. Our studies identified that a strong association between patient mortality and thrombocytopenia (platelet count <100,000/mm
3) in patients with
S. aureus bacteraemia. Using a mouse model of
S. aureus bacteremia, we identified two FDA approved drugs, the P2Y12 inhibitor ticagrelor and a sialidase inhibitor oseltamivir, which we repurposed to potently inhibit
S. aureus through blocking α-toxin platelet toxicity and Ashwell-Morell receptor mediated platelet clearance, respectively. We also examine how platelet and red blood cell membrane coated nanoparticles or "nanosponges" can act as decoys during infection to act as a novel biomimetic. Our major focus continues to investigate how platelets contribute to innate immunity in response to other bacterial pathogens. Our collaborators include G. Sakoulas (UCSD) and L. Zhang (UCSD).
Immune Signaling in Macrophages
We investigate a variety of signal transduction mechanisms and cellular pathways by which macrophages are rapidly activated in response to bacterial infection, but then able to resolve inflammation to limit collateral damage to host tissues. Areas of investigation include the roles of IKK/NFkB and MAP kinase pathways in regulating macrophage bactericidal and cytokine responses to infection, the role of transcription factor hypoxia inducible factor 1 (HIF-1a), the function of NOD-like intracellular pattern receptors in response to bacterial toxins, mechanisms of inflammasome activation and IL-1ß signaling, bacterial modulation of host cell apoptotic pathways, ATP/adenosine receptor signaling in neutrophil chemotaxis and bacterial killing, and the role of autophagy in host defense against intracellular pathogens. As a new participant of the NIH/NIAID Great Lakes Regional Center for Excellence in Biodefense and Emerging Infectious Disease Research, we are utilizing the information gained from these studies to design strategies for pharmacological enhancement of phagocytic cell function vs. antibiotic-resistant pathogens. Collaborators include Michael Karin (UCSD), Christopher Glass (UCSD) and Zev Ronai (SBMRI).
Cathelicidin AMPs in Skin Immunity
In a complex environment, higher organisms face the constant threat of microbial infection. Effective first lines of defense against infectious pathogens comprise the innate immune system. A key component of innate immunity is the production of small, cationic AMPs, a protection strategy conserved from insects through man. In a longstanding collaboration with the laboratory of Richard Gallo (UCSD), we have adopted a combined mammalian and bacterial genetic approach to decipher the contributions of the cathelicidin family of AMPs to host immunity. Our studies with cathelicidin KO mice and GAS infection provided the first in vivo demonstration that endogenous expression of a mammalian antimicrobial peptide protects against invasive bacterial infection. Ongoing collaborative projects now explore additional immunostimulatory functions of the cathelicidin molecule, its transcriptional regulation by HIF and VitD in response to infectious challenge, the molecular and phenotypic basis of bacterial sensitivity or resistance to AMP action, and the impact of bacterial AMP resistance on virulence and infectious disease epidemiology.
Other areas of research:


 Platelets, small anuclear circulating cells, are well known for their role in hemostasis. More recently, platelets have been identified as critical immune mediators in response to bacterial pathogens. Our focus examined the role of platelets during Staphylococcus aureus infection. Our studies identified that a strong association between patient mortality and thrombocytopenia (platelet count <100,000/mm 3) in patients with S. aureus bacteraemia. Using a mouse model of S. aureus bacteremia, we identified two FDA approved drugs, the P2Y12 inhibitor ticagrelor and a sialidase inhibitor oseltamivir, which we repurposed to potently inhibit S. aureus through blocking α-toxin platelet toxicity and Ashwell-Morell receptor mediated platelet clearance, respectively. We also examine how platelet and red blood cell membrane coated nanoparticles or "nanosponges" can act as decoys during infection to act as a novel biomimetic. Our major focus continues to investigate how platelets contribute to innate immunity in response to other bacterial pathogens. Our collaborators include G. Sakoulas (UCSD) and L. Zhang (UCSD).
Platelets, small anuclear circulating cells, are well known for their role in hemostasis. More recently, platelets have been identified as critical immune mediators in response to bacterial pathogens. Our focus examined the role of platelets during Staphylococcus aureus infection. Our studies identified that a strong association between patient mortality and thrombocytopenia (platelet count <100,000/mm 3) in patients with S. aureus bacteraemia. Using a mouse model of S. aureus bacteremia, we identified two FDA approved drugs, the P2Y12 inhibitor ticagrelor and a sialidase inhibitor oseltamivir, which we repurposed to potently inhibit S. aureus through blocking α-toxin platelet toxicity and Ashwell-Morell receptor mediated platelet clearance, respectively. We also examine how platelet and red blood cell membrane coated nanoparticles or "nanosponges" can act as decoys during infection to act as a novel biomimetic. Our major focus continues to investigate how platelets contribute to innate immunity in response to other bacterial pathogens. Our collaborators include G. Sakoulas (UCSD) and L. Zhang (UCSD).